| Basic Option | |
|---|---|
| Preventive Care | Nothing for covered preventive screenings, immunizations and services |
| Physician Care | $30 for primary care1 |
| Virtual doctor visits by Teladoc® | $0 for first 2 visits |
| Urgent Care Center | $35 copay |
| Prescription Drugs | Preferred Retail Pharmacy: Tier 1 (Generics): $10 copay Tier 2 (Preferred brand): $55 copay2 Tier 3 (Non-preferred brand): 60% of our allowance ($75 minimum)2 Tier 4 (Preferred specialty): $65 copay2 Tier 5 (Non-preferred specialty): $90 copay2 Mail Service Pharmacy: Available to members with Medicare Part B primary only. Visit the Medicare page for more information. Tier 1 (Generics): $20 Tier 2 (Preferred brand): $100 copay Tier 3 (Non-preferred brand): $125 copay Specialty Pharmacy: Tier 4 (Preferred specialty): $85 copay2 Tier 5 (Non-preferred specialty): $110 copay2 |
| Maternity Care | $175 inpatient $0 outpatient |
| Hospital Care | Inpatient (Precertification is required): $175 per day; up to $875 per admission Outpatient: $100 per day per facility1 |
| Surgery | $150 in an office setting1 $200 in a non-office setting1 |
| ER (accidental injury) | $175 per day per facility |
| ER (medical emergency) | $175 per day per facility |
| Lab work (such as blood tests) | $0 copay1 |
| Diagnostic services (such as sleep studies, CT scans) | Up to $100 in an office1 Up to $150 in a hospital1 |
| Chiropractic Care | $30 per treatment; up to 20 visits per year |
| Dental Care | $30 copay per evaluation; up to 2 per year |
| Rewards Program | Earn $50 for completing the Blue Health Assessment3 Earn up to $120 for completing three eligible Online Health Coach goals3 |
Overview
A copay is a set amount you pay your provider for a service. So when we say, ”$30 copay,” you pay $30. (medical emergency) 15% of our allowance. $125 per day. Covered services you receive. In this case, you would pay a $25 copay for the doctor’s ofice visit, a $25 copay for the X-ray, and either a $15 copay or 50 percent coinsurance (whichever is greater) for the generic drug. Your copays (except for prescriptions) contribute toward your out-of-pocket maximum.
Historical information about copayments can be found on the 'Historical' tab
Information about copayments proposed for members in the Adult Group with income above 106% FPL, subject to approval by the Centers for Medicare and Medicaid Services can be found in the Proposed Copay Changes section of this page. More information will be posted here when available.
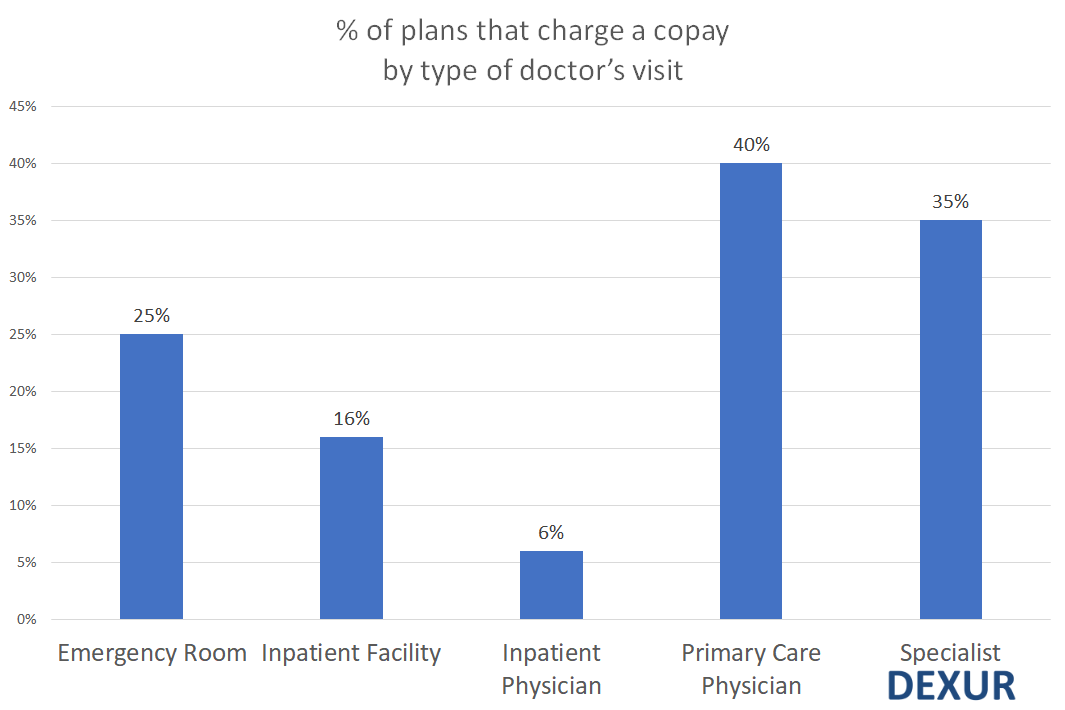
An emergency room visit typically is covered by health insurance. For patients covered by health insurance, out-of-pocket cost for an emergency room visit typically consists of a copay, usually $50-$150 or more, which often is waived if the patient is admitted to the hospital. Depending on the plan, costs might include coinsurance of 10% to 50%. A copay is a set dollar amount you pay when you get certain services or treatment. It’s part of your share of the cost for covered health care services. You pay copays directly to a provider. The only time you pay a copay is for nonemergency visits to the emergency room. Check your ID card for the amount you pay.
* NOTE: Copays under this section are copays charged under Medicaid (AHCCCS). This section does not describe copay requirements under Medicare.
Some people who get AHCCCS Medicaid benefits are asked to pay copays for some of the AHCCCS medical services that they receive. Copays can be mandatory (also known as required) or optional (also known as nominal) as explained below. Some people and certain services are exempt from copays which means that no mandatory or optional copays will be charged as explained below.
Copays are not charged to the following persons:
- People under age 19
- People determined to be Seriously Mentally Ill (SMI) by the Arizona Department of Health Services
- Individuals up through age 20 eligible to receive services from the Children's Rehabilitative Services program
- People who are acute care members and who are residing in nursing homes, or residential facilities such as an Assisted Living Home and only when the acute care member’s medical condition would otherwise require hospitalization. The exemption from copays for acute care members is limited to 90 days in a contract year
- People who are enrolled in the Arizona Long Term Care System (ALTCS)
- People who are Qualified Medicare Beneficiaries
- People who receive hospice care
- American Indian members who are active or previous users of the Indian Health Service, tribal health programs operated under P.L. 93-638, or urban Indian health programs
- People in the Breast & Cervical Cancer Treatment Program
- People receiving child welfare services under Title IV-B on the basis of being a child in foster care or receiving adoption or foster care assistance under Title IV-E regardless of age.
- People who are pregnant and throughout the postpartum period following the pregnancy
- People in the Adult Group (for a limited time*)
*For a limited time persons who are eligible in the Adult Group will not have any copays. Members in the Adult Group include persons who were transitioned from the AHCCCS Care program as well as individuals who are between the ages of 19-64, and who are not entitled to Medicare, and who are not pregnant, and who have income at or below 133% of the Federal Poverty Level (FPL) and who are not AHCCCS eligible under any other category. Copays for persons in the Adult Group with income over 106% FPL are planned and can be found on the Proposed Copay Changes tab. Members will be told about any changes in copays before they happen.
Emergency Company Notification Policy
In addition, copays are not charged for the following services for anyone:
- Hospitalizations
- Emergency services
- Family Planning services and supplies
- Pregnancy related health care and health care for any other medical condition that may complicate the pregnancy, including tobacco cessation treatment for pregnant women
- Well visits and preventive services such as pap smears, colonoscopies, and immunizations
- Services paid on a fee-for-service basis
- Provider preventable services
- Services received in the emergency department
People with Nominal (Optional) Copays

Individuals eligible for AHCCCS through any of the programs below may be charged nominal copays, unless they are receiving one of the services above that cannot be charged a copay or unless they are in one of the groups above that cannot be charged a copay. Nominal copays are also called optional copays. If a member has a nominal copay, then a provider cannot deny the service if the member states that s/he is unable to pay the copay. Members in the following programs may be charged nominal copays unless they are receiving one of the services above that cannot be charged a copay or unless they are in one of the groups above that cannot be charged a copay. Members in the following programs may be charged a nominal copay by their provider:
- State Adoption Assistance for Special Needs Children who are being adopted
- Receiving Supplemental Security Income (SSI) through the Social Security Administration for people who are age 65 or older, blind or disabled
- SSI Medical Assistance Only (SSI MAO) for individuals who are age 65 or older, blind or disabled
Ask your provider to look up your eligibility to find out what copays you may have. You can also find out by calling your health plan member services representative. You can also check your health plan's website for more information.
AHCCCS members with nominal copays may be asked to pay the following nominal copays for medical services:
| Service | Copayment |
|---|---|
| Prescriptions | $2.30 |
| Out-patient services for physical, occupational and speech therapy | $2.30 |
| Doctor or other provider outpatient office visits for evaluation and management of your care | $3.40 |
Detailed service codes and category description that comprise each of the above categories are outlined on the attached Document
Medical providers will ask you to pay these amounts but will NOT refuse you services if you are unable to pay. If you cannot afford your copay, tell your medical provider you are unable to pay these amounts so you will not be refused services.
Some AHCCCS members have required (or mandatory) copays unless they are receiving one of the services above that cannot be charged a copay or unless they are in one of the groups above that cannot be charged a copay. Members with required copays will need to pay the copays in order to get the services. Providers can refuse services to these members if they do not pay the mandatory copays. Mandatory copays are charged to persons in Families with Children that are no Longer Eligible Due to Earnings - also known as Transitional Medical Assistance (TMA)
Adults on TMA have to pay required (or mandatory) copays for some medical services. If you are on the TMA Program now or if you become eligible to receive TMA benefits later, the notice from DES or AHCCCS will tell you so. Copays for TMA members are listed below.
| Service | Copayment |
|---|---|
| Prescriptions | $2.30 |
| Doctor or other provider outpatient office visits for evaluation and management of your care | $4.00 |
| Physical, Occupational and Speech Therapies | $3.00 |
| Outpatient Non-emergency or voluntary surgical procedures | $3.00 |
Detailed service codes and category description that comprise each of the above categories are outlined on the attached Document
The amount of total copays can not be more than 5% of the family’s total income during a calendar quarter (January-March, April-June, July-September, and October-December). If this 5% limit is reached, no more copays will be charged for the rest of that quarter. AHCCCS has a process to track cost sharing. If a member thinks that the total copays they have paid are more than 5% of the family's total quarterly income and AHCCCS has not already told them, the member should send copies of receipts or other proof of how much they have paid to:
AHCCCS
801 E. Jefferson
Mail Drop 4600
Phoenix, Arizona 85034
Er Copay Meaning
If a member’s income or circumstances have changed, it is important to contact the eligibility office right away.
Emergency Copy Of Birth Certificate
NOTE: The information posted on this webpage describing proposed copays is being updated. AHCCCS is working with CMS to revise the State Plan Amendment for copays that AHCCCS plans to charge members in the future. This webpage, and the link to the revised State Plan Amendment, will include the updated changes to copays when they become available. AHCCCS will also provide additional public notice of the changes to copays that AHCCCS will be proposing to charge members.
